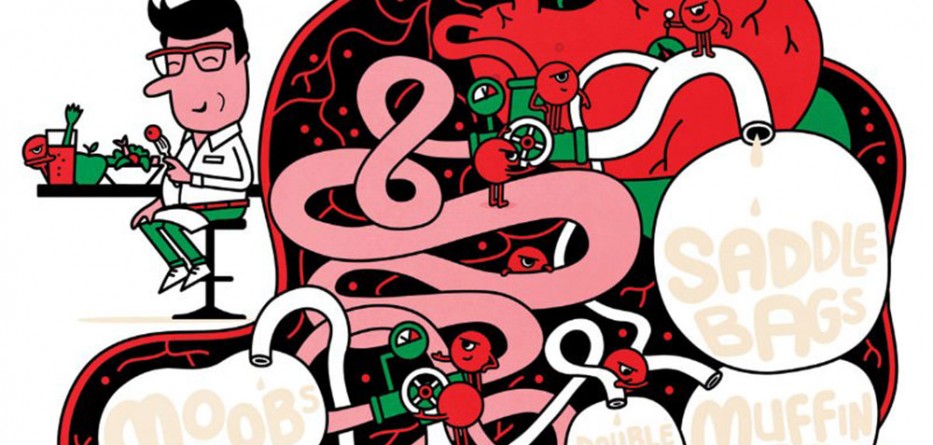
How the trouble starts
This New Scientist article, usually accessible only to subscribers, is made available for free by Philips
FOR those of us who would like to shed a few pounds, dietary advice usually boils down to brute arithmetic. Reduce energy input by eating less, and increase energy output by exercising more. Simple. Except that as anyone who has tried it knows, it isn’t.
One reason is that our evolutionary history has given us a powerful drive to eat rich foods when they are available. Now that they are virtually ubiquitous, resisting temptation can be an endless losing battle.
But there’s more to it than that. Treating food as simple units of energy – 100 calories in a chocolate-chip cookie, 1 calorie in a celery stick – may make diets easier to understand, but it is a recipe for failure. Food contains a lot more than just energy. It is stocked with powerful molecules that change how your metabolism works. The odds of meeting the infuriating demands of a calorie-controlled diet are seriously stacked against you.
The idea that the “calories in, calories out” model is too simplistic has been gaining ground for years. Many other influences seem to play a role, from the bacteria that live in your gut to how the food is cooked.
The latest findings concern the constituents of food itself. Our bodies have a finely tuned system that controls intake and determines how much we squirrel away in fat. It turns out that molecules within food can perturb this system. Some stimulate appetite and fat storage. Others do the opposite, turning on brain circuits that suppress appetite.
As a consequence, some researchers are calling for a nutritional rethink. They argue that it would be useful to think of food as being like a cocktail of hormones that influence multiple aspects of biology, including metabolism (Science, vol 339, p 918).
One of those researchers is Randy Seeley, an obesity specialist at the University of Cincinnati in Ohio. By understanding how these “nutri-hormones” work, he says, we could perhaps design diets to tip the scales in our favour. The idea could also have implications for treating illnesses linked to poor diet, such as diabetes, cardiovascular disease and even certain types of cancer. If Seeley is right, nutrition science is on the brink of a new era.
Hormones and food have always been intimately linked. Hormones are the body’s chemical messengers, manufactured by specialist cells and dispatched into the bloodstream towards distant destinations. One of the first to be discovered was insulin, which the pancreas produces in response to a meal to instruct liver, muscle and fat cells to pull glucose out of the bloodstream.
Most hormones deliver their message by docking with receptors on the surfaces of cells, triggering a cascade of metabolic reactions inside. Others slip into the cell and interact with receptors within the nucleus, controlling gene expression, for example.
Hormones were once thought to be an exclusive group of molecules manufactured by specialist glands such as the pancreas and thyroid. But the hormone club has become much more inclusive as we have discovered a labyrinthine network of signalling molecules and receptors – many of them involved in energy metabolism. In 1995, for example, a team at Rockefeller University in New York City discovered leptin, which is made by fat cells and activates receptors in the brain to suppress appetite.
Around the same time, other scientists saw the first signs that food itself could directly influence the body’s energy-control networks. In the early 1990s, researchers discovered that a common but mysterious class of receptor in the cell nucleus, called peroxisome proliferator-activated receptors, or PPARs, could be switched on by fatty acids.
We now know that these receptors play an important role in energy balance. Nobody has discovered a hormone that binds specifically to them and it now seems that their job is to sense a wide range of fatty acids and other molecules involved in fat metabolism. “These receptors were designed to listen to the food,” says Seeley.
Store more fat!
They don’t just listen – they talk back. One type, PPAR-gamma, is found in fat cells. When fatty acids bind to it, the receptor switches on genes that make new fat cells and promote fat storage. It also cuts production of another key messenger in energy metabolism called uncoupling protein-1, which tells cells to burn fat for heat. Less uncoupling protein-1 means that more food is laid down in fat stores. Not surprisingly, activating the PPAR-gamma receptor fattens up mice, while switching it off has the opposite effect.
In other words, eating a high-fat diet doesn’t just stuff you full of calories – it tilts your metabolism towards obesity. “You’re subtly changing the biology of how the body stores fat,” says Seeley.
“A high-fat diet doesn’t just stuff you full of calories, it tilts your metabolism towards obesity”
It gets worse. The receptors are also found in brain cells. Jerrold Olefsky of the University of California, San Diego, has shown that when mice are fed a high-fat diet, their weight gain is partly due to the action of these receptors. Activating them with drugs made the mice consume more calories and gain twice as much body fat as control animals.
Olefsky and Seeley also found that damping down PPAR-gamma activity in mice can cause weight loss even when the mice eat a high-fat diet – although it required genetic tinkering. Blocking the receptor with drugs could offer a more acceptable route to the same effect for a human dieter, suggests Seeley.
The signals that fatty acids carry are not all bad news. You’ve probably heard of omega-3 fatty acids. They are widely touted as having health-giving properties and there is some evidence that consuming them can reduce the risk of coronary heart disease and obesity.
The most prized are docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), which the human body has limited ability to make and so depends on dietary sources such as fatty fish, seeds and nuts. “We already know that omega-3 fatty acids have [positive] long-term consequences for health,” says Seeley. The big question is: why?
The answer seems to lie in their hormone-like properties. In 2010, Olefsky’s team discovered that both molecules bind tightly to a cell-surface receptor called GPR120, which is abundant on fat cells. This receptor has an enormous influence on metabolism. Reduced GPR120 activity is linked to inflammation, weight gain and poor control over blood sugar. Last year, researchers found that obese people were more likely to have a genetic fault in their GPR120 receptors.
Until recently, GPR120 was regarded as an “orphan” receptor, meaning that the hormone that binds to it had not been discovered. But now it seems that its job is to respond to omega-3s in food – another piece of evidence that there is more to obesity than simple calorie arithmetic.
For most people that merely emphasises the importance of eating a balanced diet. But for a few unlucky ones it is more serious. According to one study, roughly 3 per cent of people have a GPR120 mutation, giving them a 60 per cent higher risk of obesity. The conclusion, says Philippe Froguel at Imperial College London, who discovered the mutation, is that if you do not eat healthily, small genetic disadvantages can have a big effect. “The effect of genes is magnified by your way of life,” he says.
GPR120 receptors are also considered prime targets for pharmaceuticals that could help to stop the proliferation of obesity. “All drug companies have some sort of project on this,” says Frank Reimann at the Cambridge Institute for Medical Research in the UK.
Food’s hormone-like properties do not just belong to fat. Amino acids – the building blocks of proteins – can also affect appetite pathways. Seeley has investigated a protein called mTOR, which normally acts as a sensor for ATP – the main energy currency of the cell. Seeley says that mTOR’s job is to monitor energy and nutrient levels and decrease food intake if there is a surplus.
He found that the amino acid leucine can switch on mTOR, making mice eat less. It is possible that diets packed with this compound could damp down your appetite – which should be pretty easy to implement. “Most high-protein foods have lots of leucine; foods such as soya beans, eggs, peanuts, meat and fish,” says Seeley. “There have been rodent tests of high-protein diets that reduce weight.”
Another interesting amino acid is glutamine, which Reimann has found to be particularly effective at stimulating release of an appetite-suppressing hormone called glucagon-like peptide-1 – another possible reason why high-protein diets work.
Carbohydrates, too, are proving able to tweak metabolism in interesting ways. Complex carbohydrates like starch and cellulose are processed by gut microbes into short-chain fatty acids, which then bind to receptors on specialised cells in the gut. These cells respond by releasing glucagon-like peptide-1.
Slimline surgery
That is just a part of the normal system for sensing energy intake and modulating it. But for Froguel there’s likely to be more to it than that. “The next frontier is carbs,” he says.
This interplay between food, gut microflora, hormones and receptors may even explain the success of the gastric bypass surgery used to treat some very obese people. It involves re-plumbing the gut so that food takes a shortcut from the stomach to the small intestine. But simply reducing the volume of the digestive system cannot explain its effect, says Seeley.
Instead, the surgery drastically changes the make-up of the microbes in the gut, which leads to an increase in the amount of appetite-suppressing glucagon-like peptide-1 being released. “The microbes change; the hormone profile changes too,” says Reimann.
This suggests that there may be less drastic ways to achieve the same results using food molecules, he adds. “We’re working towards methods to modify the release of hormones without surgery.”
Translating this basic biology into a healthy diet remains a hope rather than a reality. “In general, the public – and even nutritionists – don’t look at food as having these kinds of regulatory molecules,” says nutrition scientist Donald Jump of Oregon State University in Corvallis.
But it is early days for the idea, and there could be many more discoveries to come. “In the long run it could be incorporated into diet advice,” agrees Reimann. Seeley even anticipates that diets could become much more personalised, based on individuals’ responses to the hormone-like molecules in food. “The ‘right diet’ isn’t the same for everyone,” he says.
That’s not to say that calories no longer matter. But they might just matter a little less than they used to. I’ll eat to that.
Source: newscientist.com









whoah this weblog is magnificent i really like studying your articles.
Stay up the great work! You realize, many people are searching around for this information, you could
aid them greatly.